Improvement Needed STAT: Linkage to HIV Care
Topics
Ask yourself this question: “How long would I want to wait to see a doctor if I was told I had HIV or another potentially life-threatening infection?”
It’s understandable that people who have just been diagnosed with HIV don’t want to have to wait for weeks to see a doctor who is experienced treating the infection. A delay of a few weeks or a month wouldn’t make a significant difference in their long-term health or survival. It does, however, make a difference when it comes to the mental health of people living with HIV and reducing the length of time that people who are newly diagnosed have a detectable viral load and are at greater potential risk of transmitting the virus.
We believe that it also sends a strong and clear message that gets their HIV care off to the right start. It reinforces messages about the seriousness of HIV infection and the value of HIV treatment. It allows for health care relationships to be established between people living with HIV and health care providers at a critical time. This allows the health care provider to start the healing process by addressing the stress, answering the questions, and letting the person living with HIV know that they will be cared for and will be ok.
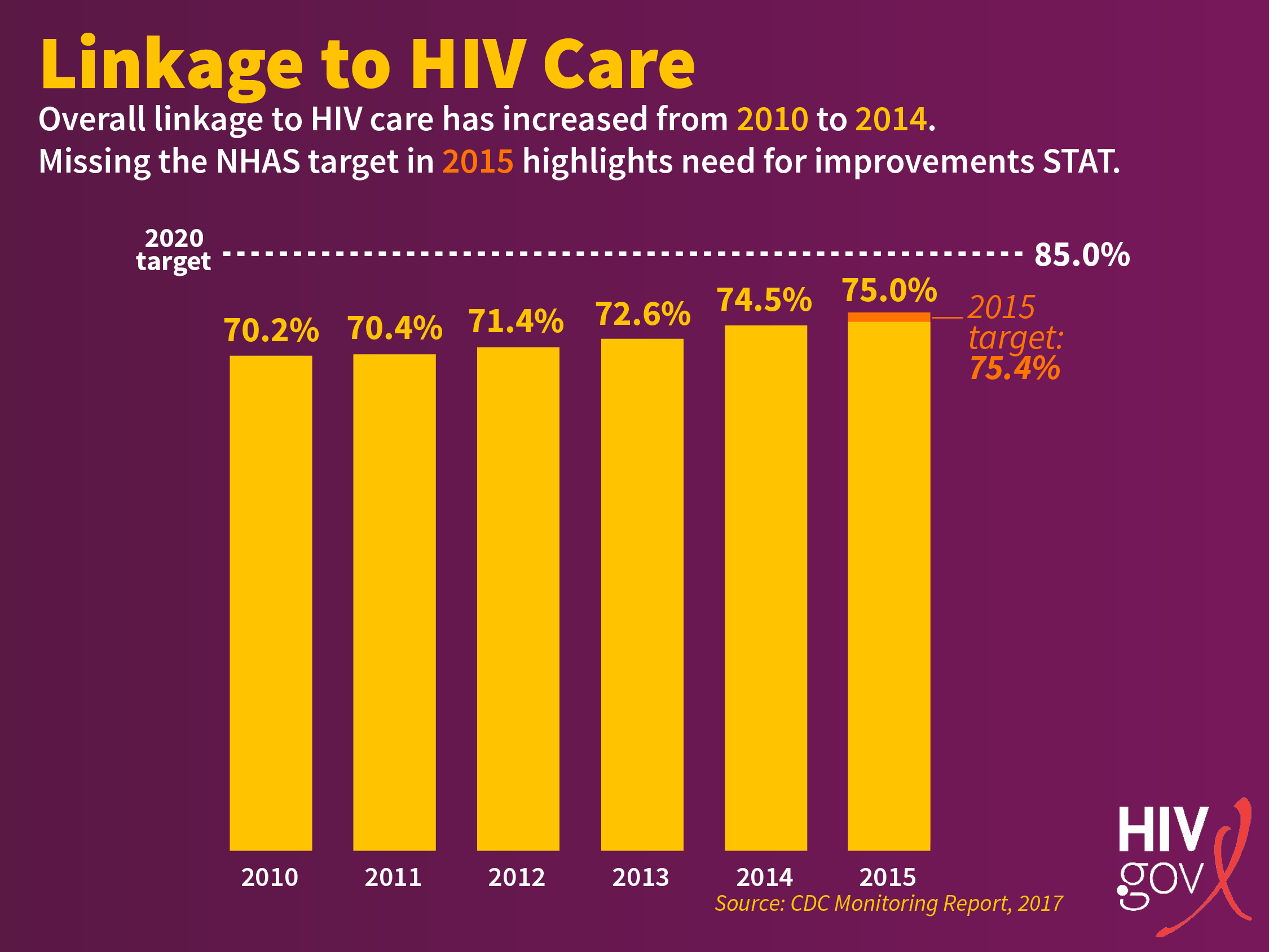
While the proportion of those linked to care [within 30 days of HIV diagnosis] has steadily increased since 2010, we missed our annual target for 2015 (75.4%)…Missing the 2015 annual target is a warning sign that we are at risk of missing the 2020 target (85%).
The National HIV/AIDS Strategy sets our target for increasing the percentage of newly diagnosed persons linked to HIV medical care within one month of diagnosis to at least 85% by 2020. According to the most recent data available in the Monitoring Report [PDF, 2,374 KB] from the Centers for Disease Control and Prevention (CDC), in 2015 75% of people diagnosed with HIV were linked to HIV medical care within one month after diagnosis. While the proportion of those linked to care has steadily increased since 2010, we missed our annual target for 2015 (75.4%) by only 0.4%. Missing the 2015 annual target is a warning sign that we are at risk of missing the 2020 target (85%). The 2015 target required a 10% increase from the 2014 target in the number of people newly diagnosed with HIV who were linked to care. The annual targets will escalate to 15% increases for 2018-2020 to meet the 2020 target.
CDC monitors linkage to HIV medical care using laboratory data from areas with complete reporting of CD4 and viral load tests. The CDC defines linkage to HIV care as receiving a CD4 or viral load test within 1 month after diagnosis. The 2015 indicator data is based on reporting from 38 jurisdictions, an increase from 14 in 2010. Data from these 38 jurisdictions represent 71.9% of all persons aged ≥13 years living with diagnosed HIV at year-end 2014. To assess changes in linkage to care and account for the changes in the number of jurisdictions contributing data, the CDC also assesses trends in linkage to care for jurisdictions included at baseline that contributed data for each year of the assessment. The number of jurisdictions reporting these data are expected to increase in coming years, providing a better representation of the nation as a whole.
Reviewing the data further, there are concerning disparities in linkage to HIV care among people diagnosed with HIV in 2015. People ages 13-24 have the lowest rates of linkage to HIV care (70.5%). In addition, it is also important to look at all the groups that we missed the 2015 target for: only 73.9% of people ages 25-34, 71.3% of Blacks, 73.7% of Native Hawaiians and Pacific Islanders, and about 71% of people who inject drugs were linked to HIV care within one month of diagnosis in 2015.
Progress across the HIV care continuum is necessary for getting people living with HIV virally suppressed to protect their health and stop new HIV infections. Not meeting our national targets will mean poorer health among people living with HIV and additional infections that could have been prevented.
Linkage to care is critically important in the fight against HIV. It is an essential and required part of the service provided by programs that perform HIV testing. Every person who is not linked to care within 30 days is a missed opportunity and negates a fundamental purpose of testing. The lack of major improvement in this indicator is worrisome given the emphasis that has been put on linkage and may indicate organizational challenges, limited or strained clinic capacity, and other logistical challenges in moving people to care.
It also likely indicates that we are still burdened by the baggage of the very early days of the epidemic when treatment wasn’t particularly effective and in most cases toxic for those who took them. At that time, HIV care was mainly for those who developed symptoms of and were dying from complications of AIDS. Even when effective treatments became available in the mid-1990s, treatment guidelines didn’t recommend treatment for all people living with HIV until 2012. Subsequently, results from the Strategic Timing of AntiRetroviral Treatment (START) and TEMPRANOExit Disclaimer studies, which looked at optimal time to begin treatment, led to the recommendation that all patients, regardless of CD4 cell count begin treatment immediately upon diagnosis. This is a huge change; but not everyone has caught up to this change yet.
Our lack of progress in linkage to care in 2015 is also an indication of the multiple challenges that people with HIV face. Among others, lack of employment, housing, and access to care create barriers to starting (and remaining in) care for many people living with HIV. In addition, the denial and shame that HIV stigma can trigger prevents some people from accessing care.
To meet the 2020 NHAS goals much more must be done. The CDC Compendium of Evidence-Based Interventions and Best Practices for HIV Prevention includes a number of best practices in promoting linkage to, retention in, and re-engagement in HIV care among people living with HIV. Clear referral protocols must be developed and implemented to facilitate quick access to care after a confirmed positive HIV test. We must continue to build the capacity and cultural competency of the HIV workforce. We must build the relationships, the protocols, the capacity and the commitment to make it possible for all people who are diagnosed with HIV to immediately enter HIV care. If we can do this well, our job will be much easier at each and every subsequent step along the continuum, we will have fewer new infections, and fewer HIV-related deaths.
In the next post in our continuing NHAS Indicators series, we will look at the indicator highlighting retention in HIV care. Stay tuned…