SMAIF In Action: Health Models Program in Louisiana Improves HIV Viral Suppression In All Three Participating Clinics
Topics
Three clinics in Louisiana implemented the Health Models program with support of the Secretary’s Minority AIDS Initiative Fund (SMAIF) and saw viral suppression among people living with HIV increase at each participating clinic.
It is essential that every person living with HIV be in medical care and receive effective HIV treatment for their entire life (or until a cure is found). This keeps them healthy and reduces the possibility that they would be able to pass on HIV to others. The reality is, however, that keeping up with medical appointments, lab tests, and prescription refills is not always easy. Sometimes individuals experience events that make it difficult or impossible for them to stay in medical care. Not being able to take time off of work, transportation issues, a sick child, loss of insurance, inability to pay copays, mental health issues, stigma and shame can all negatively affect a person’s ability to stay engaged in HIV care. The challenges accessing HIV medical care impact the health of individuals as well as results for the states or the nation as a whole. Because these challenges (and the resources available to cope with them) are not equally distributed, challenges can affect some groups more than others, including racial and ethnic minorities, people living in the southern states, and those living in rural areas.
The Louisiana Department of Health received SMAIF funding as part of the Care and Prevention in the United States (CAPUS) demonstration project to improve HIV screening, linkage and retention in care, and health outcomes—like viral suppression—for racial and ethnic minorities living with HIV. In order to maximize the impact of this investment, they established the Health Models program to focus on three areas with a high density of HIV infection: Marrero, New Orleans, and Baton Rouge. The program began in September 2013 and combined multiple approaches to increase the number of people living with HIV in those communities who achieved and sustain viral suppression. Health Models used public health surveillance data to find people living with HIV who had dropped out of care, worked to bring them back into care, and provided treatment adherence counseling. This was coupled with financial incentives to engage individuals in HIV medical care with the ultimate goal of having the individual attain and maintain viral load suppression. Engaging people in HIV medical care and maintaining viral load suppression are essential for stopping HIV from further damaging the immune system and for preventing transmission to others. The ability of HIV treatment that leads to viral suppression to stop HIV from being transmitted sexually is one the biggest scientific breakthroughs in the past few years. That’s why treatment is so important for keeping HIV-negative people free from HIV.
“HIV treatment is still [too] expensive, and the burden of HIV is still faced…by a population who has extremely limited financial resources.”
-Health Models Project Manager
The incentives and adherence counseling delivered by the Health Models program are working for the clients who are enrolled in the program. The incentives increase from $10 to $75, as clients complete various events that ultimately lead to viral load suppression. These incentives are modest compared to the costs of changing drug regimens or treating HIV that has progressed because clients have dropped out of care or are not consistently taking their medication. The financial incentive is often used to address barriers to care, such as paying for household bills, transportation, food, medication, and medical copayments. Some clients also use the funds for purchases unrelated to their HIV treatment. Removing financial barriers and giving clients the freedom and power to make the decision on how to use their incentives allows them to take control of their participation in the program and their HIV medical care.
Health Models care coordinators provide treatment adherence counseling and focus on helping clients understand their viral load, the importance of staying in care and not missing medication doses, and how treatment adherence affects their lab test results and their overall good health. While clinics offer numerous opportunities for clients to acquire health information, the Health Models encounter is solely focused on viral suppression and giving the client the knowledge and supportive services needed to achieve and maintain it.
Health Models clients show signs of having become more empowered with regards to their health. Clinic staff and administrators indicate that the project has resulted in a slightly lower “no-show” and appointment cancellation rates among clients of about 3%. There has also been an increase in clients initiating conversations about their lab results and health status during provider visits. But it is the changes in viral suppression that truly show the power of the Health Models program.
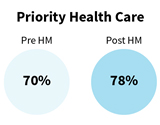
The objective of successful HIV treatment is viral suppression to a level that HIV is no longer detectable with standard lab tests. It is essential for all people living with HIV to achieve and maintain viral suppression to maximize the benefits of HIV treatment, prevent disease progression, and prevent transmission to others. Beginning in 2013, the Health Models program was able to successfully achieve viral load suppression for the majority of the 2,066 enrollees during the program period. All of the participating clinics showed improvement in the proportion of clients who achieved viral suppression from the period before initiation of the Health Models program compared to after implementation of the program. Preliminary results showed that clinic improvements in viral suppression ranged from an increase of about 5 to 8 percentage points in a little over two years. Pre- and post-Health Models implementation viral load suppression rates were: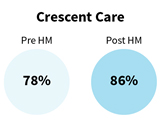

The SMAIF-funded Health Models program has transformed the clinics’ protocols for HIV treatment adherence in Louisiana. Due to the effectiveness and impact of the Health Models intervention, the program is now using core HIV funding to the state health department from the Centers for Disease Control and Prevention (CDC) to continue the program as part of its standard of care in these clinics and at an additional three sites in Louisiana.
Next week, we’ll share a story of how Health Models positively impacted one of its clients.
SMAIF improves HIV prevention, care, and treatment for racial and ethnic minorities through innovation, systems change, and strategic partnerships and collaboration. SMAIF supports 33 projects in 40 states, D.C., Puerto Rico, & Guam that are conducted by 200+ health departments, health centers, and community organizations. For more information on SMAIF and the activities it supports across the country visit HIV.gov/smaif.