CDC Releases New Data from the Medical Monitoring Project
Topics

On July 12, the Centers for Disease Control and Prevention (CDC) published data from the 2020 cycle (June 2020–May 2021) of the Medical Monitoring Project (MMP). MMP is an annual, cross-sectional complex sample survey that reports nationally representative estimates of behavioral and clinical characteristics of adults with diagnosed HIV infection in the United States. This report provides information that is critical for achieving the goals of the National HIV/AIDS Strategy (NHAS) and the Ending the HIV Epidemic in the U.S. initiative. For instance, NHAS highlights the importance of addressing social determinants of health in improving HIV care and treatment outcomes and decreasing disparities in priority populations. MMP provides data on two important social determinants of health, homelessness and HIV-related stigma, to monitor progress in achieving national HIV prevention goals.
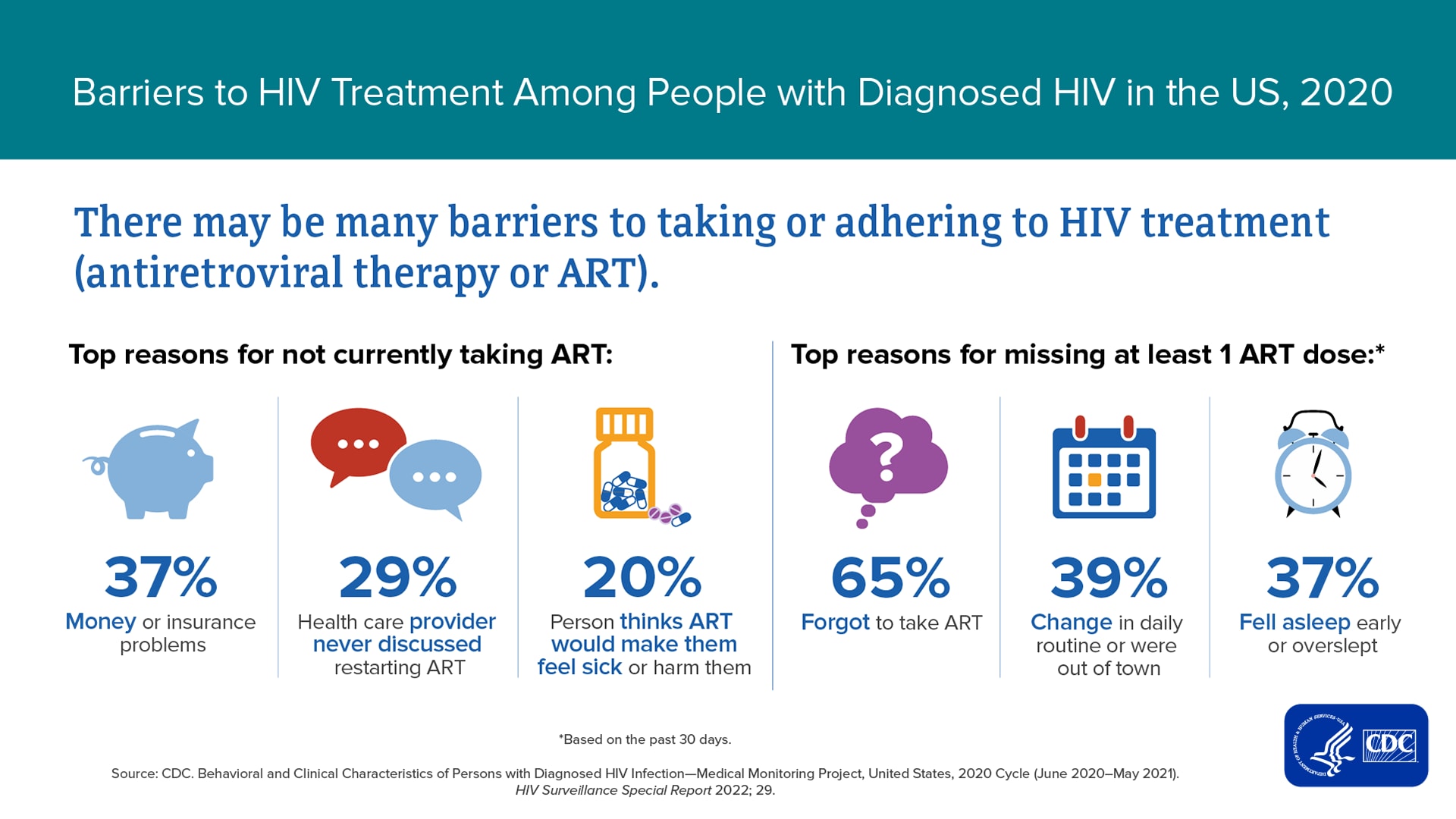
Receiving routine HIV medical care and taking antiretroviral therapy (ART) as prescribed are essential for maintaining viral suppression. The latest MMP report, based on the 2020 data cycle, shows that 80% of adults with diagnosed HIV did not miss any HIV medical appointments during the past 12 months, 95% were currently taking ART, and 62% took all prescribed ART doses during the past 30 days. Some adults with diagnosed HIV have experiences that complicate HIV care or treatment, thus making it harder to maintain viral suppression. For example, top reasons for not currently taking ART included: money or insurance problems (37%), the health care provider never discussed restarting ART (29%), or the person thought ART would make them sick or harm them (20%).
In addition, some adults with diagnosed HIV experienced socioeconomic challenges, engaged in certain behaviors, and had medical issues associated with lower levels of viral suppression. The latest MMP report shows that during the past 12 months, 17% of adults with diagnosed HIV experienced homelessness or other forms of unstable housing (8% experienced homelessness, 12% moved in with other people due to financial problems, 8% moved two or more times, and 2% were evicted from housing [not mutually exclusive measures]); 16% experienced food insecurity; and 36% were living in households <100% of the federal poverty level. An estimated 98% had health insurance or coverage for care or medications. Specifically, 47% had coverage through the Ryan White HIV/AIDS Program; 43% had Medicaid; 28% had Medicare; and 40% had private health insurance (not mutually exclusive categories). Among adults with diagnosed HIV, 15% engaged in binge drinking during the past 30 days, and 33% used drugs for nonmedical purposes during the past 12 months. An estimated 40% had a disability; 14% had symptoms of major or other depression; and 18% had symptoms of mild, moderate, or severe anxiety during the past two weeks. On a scale that ranged from 0 (lowest stigma) to 100 (highest stigma), the median HIV stigma score during the past 12 months among adults with diagnosed HIV was 28.4. The study demonstrated that although some people with HIV need ancillary services to address socioeconomic factors, behaviors, or medical issues they may experience, their needs for services are not always met. Overall, 41% of adults with diagnosed HIV had a need for at least one ancillary service that was not met, including for dental care (21%), SNAP/WIC (10%), and shelter/housing services (8%).
For more information on these findings from MMP, please see the full report.